So, you just did an IVF cycle and have a bunch of embryos that made it to blastocyst! Some are good quality, some are fair, and some are poor quality. You’ve decided you want to do preimplantation genetic testing for aneuploidy (PGT-A). You assumed that the good-quality embryos would come back as euploid, but you’re surprised to learn that some of the poor-quality embryos have tested normal, and some of the good-quality embryos have tested aneuploid. What’s going on?
“Never mind that!” everyone tells you. “Grades don’t matter if the embryo is euploid!”
So is this true?
Before we answer that question, let’s explain the difference between embryo grading and PGT-A.
What is embryo grading?
Embryo grading is a way for the embryologist to pick out the best embryo to give you the best possible chance of achieving a pregnancy. Simply put, it's a selection tool.
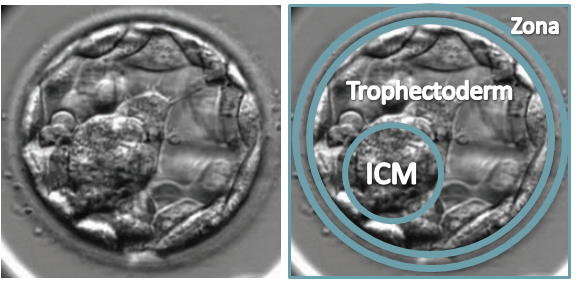
There are certain features that an embryologist looks at when assessing an embryo. These features are mainly based on the number of cells that an embryo has in its inner cell mass (ICM) and in its trophectoderm. The ICM eventually becomes the fetus, and the trophectoderm eventually becomes the placenta.
You can see what these structures are in the image below:
Credit: Remembryo.
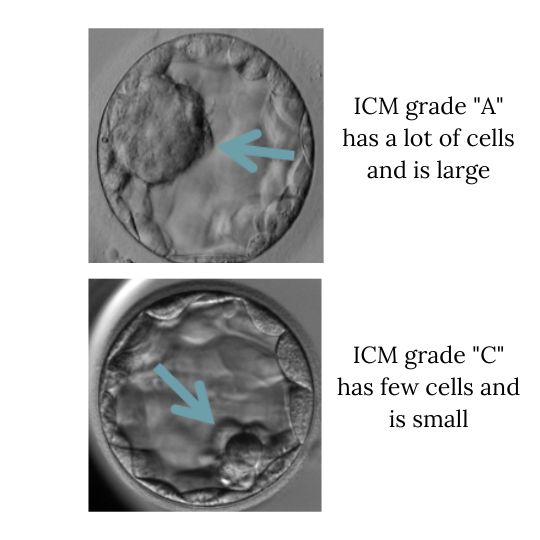
An embryo with a lot of cells in its ICM will get an “A” for its ICM quality, but one with only a few cells will get a “C.” Check out the example below to see this in action:
Adapted from Remembryo.
The trophectoderm is assessed in a similar way, and an embryo with a "good" grade typically has a lot of cells for its ICM and trophectoderm.
Several studies have shown that good-quality embryos have a higher chance of achieving pregnancy compared to embryos with lower quality. This is why embryologists grade embryos — because it gives them a ranking order for which one(s) to transfer first.
Like embryo grading, PGT-A is an embryo selection tool. But instead of looking at the embryo’s ICM and trophectoderm, it takes a closer look at the embryo’s chromosomes.
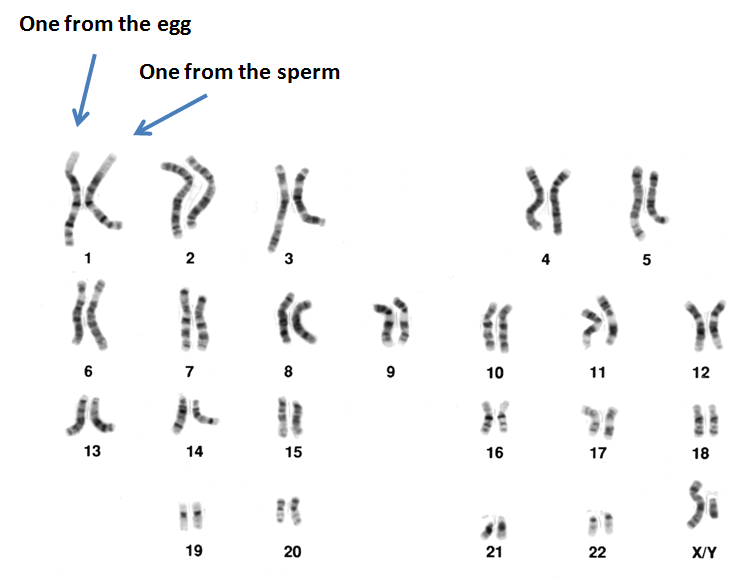
Most cells in our body contain DNA, and our DNA is packaged into structures called chromosomes. Humans have 23 pairs of chromosomes, or 46 in total, with one set of 23 coming from the egg and the other set of 23 coming from the sperm.
Credit: Remembryo.
Having the correct number of chromosomes is important. For example, an extra copy of chromosome 21, known as trisomy 21, is an abnormality commonly found in people with Down Syndrome. A monosomy is when there is only one copy of a chromosome.
Questions Women Are Asking
When PGT-A is done, about 5-10 cells are removed from the embryo’s trophectoderm during a biopsy. The cells are then transferred to a tube and shipped to a PGT-A testing lab, where the DNA is extracted to determine the number of chromosomes in the embryo’s cells.
If the cells in the biopsy sample contain 23 pairs of chromosomes, then the embryo that the biopsy came from is considered euploid, or normal. If there’s any other number of chromosomes, then the embryo is aneuploid. Besides the actual number of chromosomes, different pieces of the chromosome, or segments, can be deleted or copied. This is known as segmental aneuploidy. Translocations can also occur, where segments are moved to another location, either on the same or on a different chromosome. These are all examples of chromosomal abnormalities.
Research has shown that euploid embryos are more likely to lead to a live birth compared to aneuploid embryos, which for the most part result in implantation failure or miscarriage. Moreover, transferring an aneuploid, or abnormal, embryo is generally avoided due to the potential risk of a baby being born with a genetic disorder.
So, embryo grading and PGT-A are looking at two separate things. But together, they can provide a valuable picture of the potential for an embryo to result in a live birth.
Are embryo grading and euploidy related?
In other words, are good-quality embryos more likely to be euploid, and are poor-quality embryos more likely to be aneuploid?
Yes! One study showed that the odds of a good-quality embryo being euploid are about three times higher than a poor-quality embryo and about 1.7 times higher than a fair-quality embryo. Another study found that good-quality embryos are more likely to be euploid.
But the reality is that not all good-quality embryos result in a euploid embryo, and not all poor-quality embryos result in an aneuploid embryo. So, there are other factors besides the number of chromosomes that determine an embryo’s quality.
Now let’s look back at our original question:
Does embryo grading still matter with PGT testing?


LATESTFeb 19, 2026
Hot Take: We Should Stop Asking People If They’re Done Having Kids
“So are you done having kids?” is pretty much a standard conversational question — like, to the point that it often comes up the... READ MORE
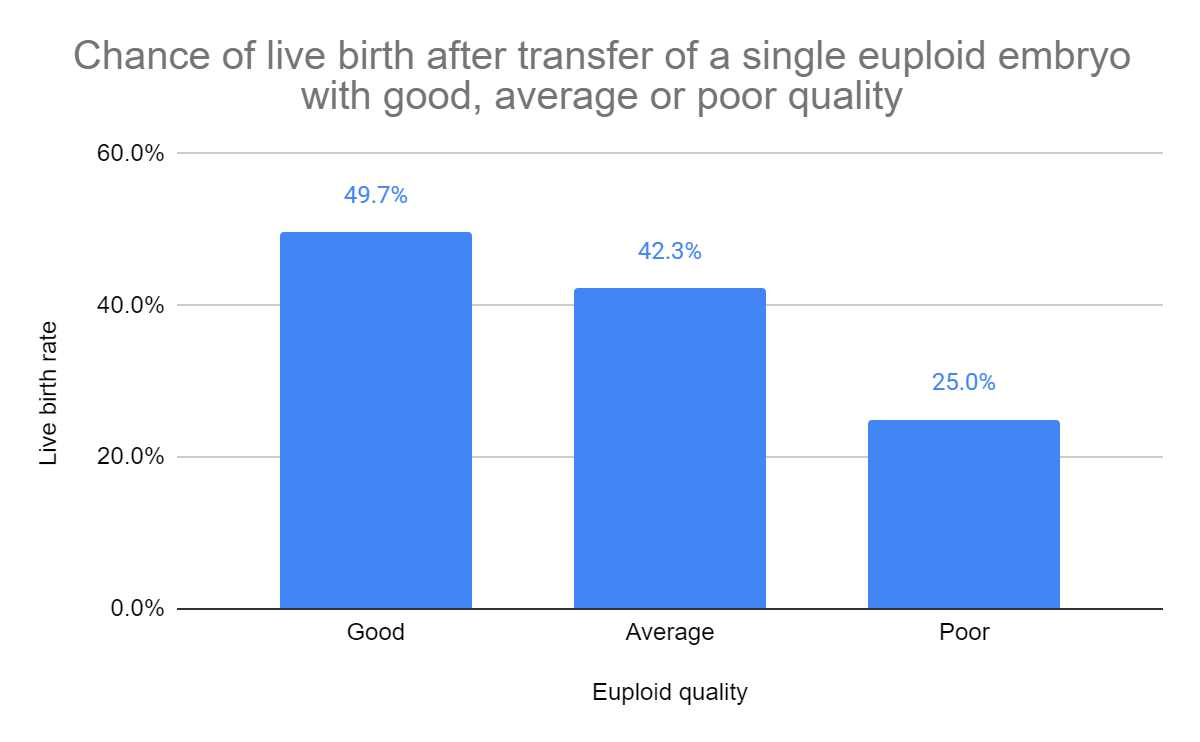
A number of studies have shown that embryo grades do still matter after PGT-A. This one found that good, fair, and poor-quality euploid embryos had live birth rates of 49.7%, 42.3%, and 25.0% respectively; and this one found that euploid embryos with a C-quality ICM had about one-third of the odds of live birth compared to a blastocyst with an A-quality ICM.
Credit: Remembryo.
You may also be surprised to learn that the day the blastocyst is biopsied, either on day 5, 6, or 7, also has an impact on a euploid embryo's success rates. This study found that day-5 euploid embryos have a higher chance of live birth compared to day-7 euploids. The same study also found that day-5 embryos are more likely to be euploid compared to day-7 embryos.
So as far as a euploid embryo goes, the quality and the day it was biopsied both play a role in transfer success rates.
Dr. Charlene Alouf, Medical Liason at Genomic Prediction, explains: “There is an array of embryo grades that have been found acceptable to perform a biopsy and within each grading designation there is a range of morphologies (e.g. not every 4AA is identical). Some studies have reported that there is a correlation between euploid rates and embryo quality; in addition to the day of biopsy (day 5, 6, or 7). What is certain is that not every high-quality embryo is normal and not every ‘poorer’ quality embryo is abnormal. Until artificial intelligence for embryo selection is refined, leading to higher sensitivity and specificity, embryo grades will continue to matter when it comes to selecting the embryos to biopsy, or rebiopsy if needed, and prioritizing the euploid embryos for transfer.”
Remember, PGT-A is a selection tool, just like embryo grading. Both of these tools look at different characteristics of an embryo, and both can be useful in determining the best embryo to transfer in hopes of a successful pregnancy.






.jpeg)

.jpeg)

.jpeg)
.jpg)







.jpg)

.png)


